Anticoagulation
Stopping anticoagulants prior to a procedure
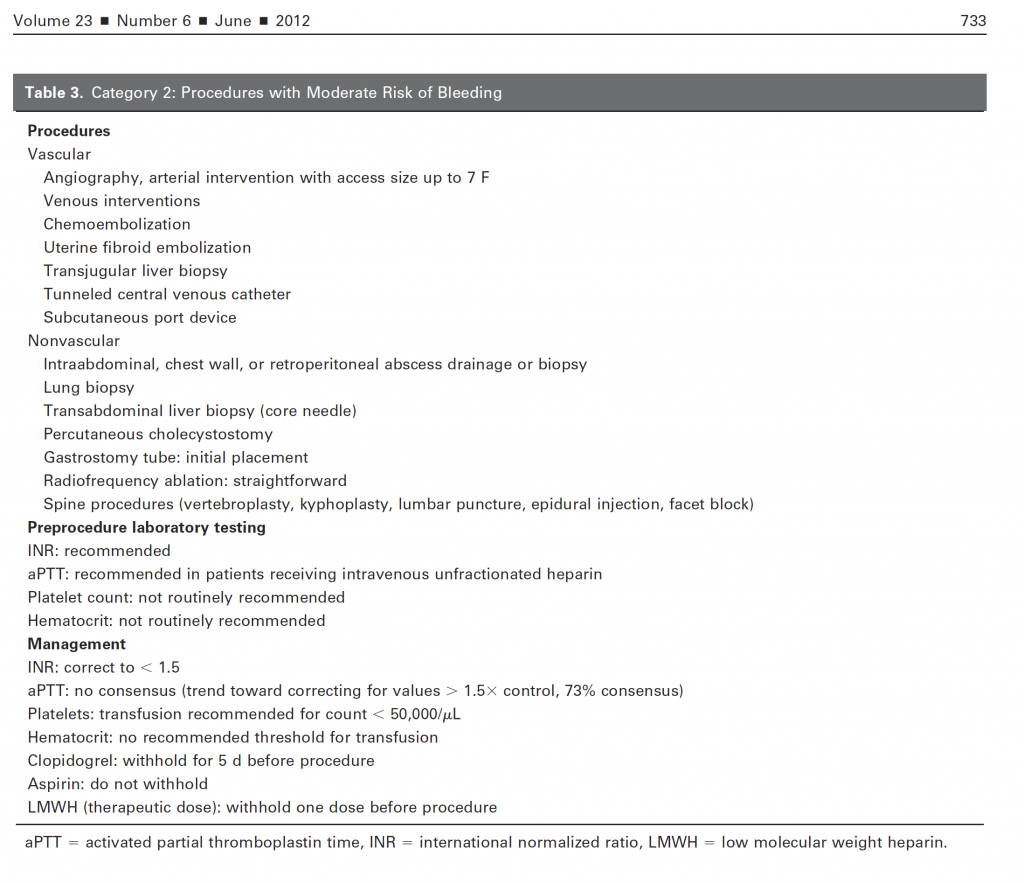
Of course, in the modern era, the greatest risk of anticoagulation arises from drugs being given to the patient. Moreover, the number of novel anticoagulants has clouded the picture further. However, recommendations for the most common anticoagulants is relatively straightforward.
- Heparin infusion: stop for 4 hours and recheck aPTT prior to beginning procedure
- Low molecular weight heparin (Lovenox): withhold one dose before procedure
- Coumadin – withhold 5 days prior to procedures, bridge according to patient’s condition
- Aspirin/NSAIDs – do not withhold
- Clopidogrel (Plavix) – withhold 5 days prior to procedures
It is of note that most studies have found no increased risk of procedural bleeding on aspirin (either 81 mg or 325 mg dose), and most experts do not recommend stopping aspirin prior to a procedure.
Anyone who has seen TV commercials lately knows there has been a proliferation of new oral anticoagulants, including Pradaxa, Xarelto, Eliquis, and Savaysa. The use of these anticoagulants complicates the issue considerably because they are often slowly cleared and have no reversal agents. For this reason, they must frequently be stopped anywhere from 3-5 days prior to a procedure. Prior to performing a procedure on a patient on advanced anticoagulant, consulting your institution’s policies is recommended.
Finally, these recommendations are only suggestions to help in the best management of the patient. Some patients may be at slightly higher risk because of the difficulty of the procedure or other complications. Additionally, the risk of bleeding is likely additive when patients are on more than one medication with anticoagulation or antiplatelet effects, and that additional risk should be considered.
In conclusion, it is possible to perform procedures on patients with coagulopathy and on anticoagulants, but they should be performed with knowledge of the risk involved and while taking steps to minimize that risk.