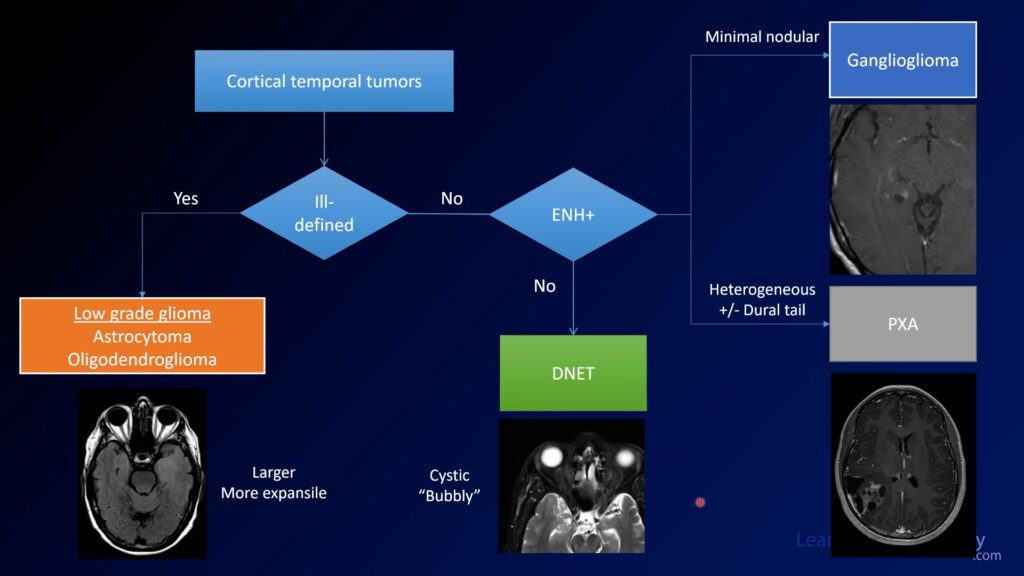
Neuroradiology Board Review – Brain Tumors – Case 14
Neuroradiology brain tumor board review. This lecture is geared towards the ABR core exam for residents, but it would be useful for review for the ABR certifying exam or certificate of added qualification (CAQ) exam for neuroradiology.
More description and the answer (spoiler!) are seen below the video.
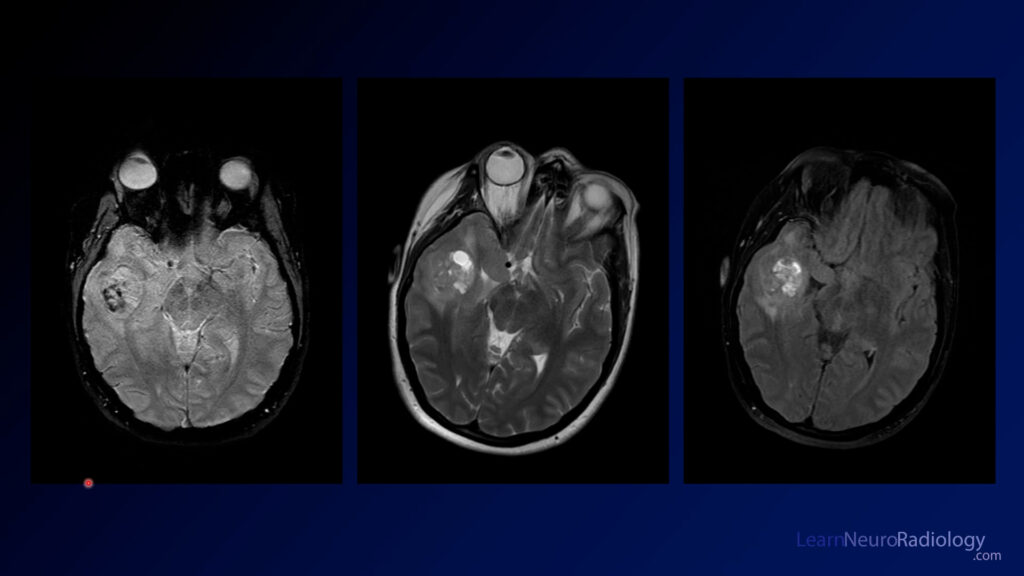
This case shows an MRI with a mass in the left parietal region near the midline. It is pretty well circumscribed and is probably extra-axial. It is homogeneously enhancing on postcontrast, and both T2 and T1 images demonstrate significant vascular flow voids suggesting that this is a very vascular lesion.
The diagnosis is: solitary fibrous tumor
Solitary fibrous tumors of the CNS (previously known as hemangiopericytomas) are similar in histology to fibrous tumors elsewhere in the body, such as the pleura. These were originally thought to be related to meningiomas, but their genetics has proven this to be false. However, the imaging features are similar to aggressive meningiomas. They are most often extra-axial, have avid enhancement, and broad dural attachments. It is common to have flow voids showing a high degree of vascularity.
Like meningiomas, these can be highly vascular lesions with much of their blood supply coming from external carotid branches. This angiogram shows the high degree of vascularity. It can be favorable to embolize as many of these vessels as possible prior to surgical resection to minimize bleeding.
Remember that the nomenclature has changed but you still may run into the term hemangiopericytoma. It’s something that should be on your differential if you see something that looks like an aggressive meningioma.